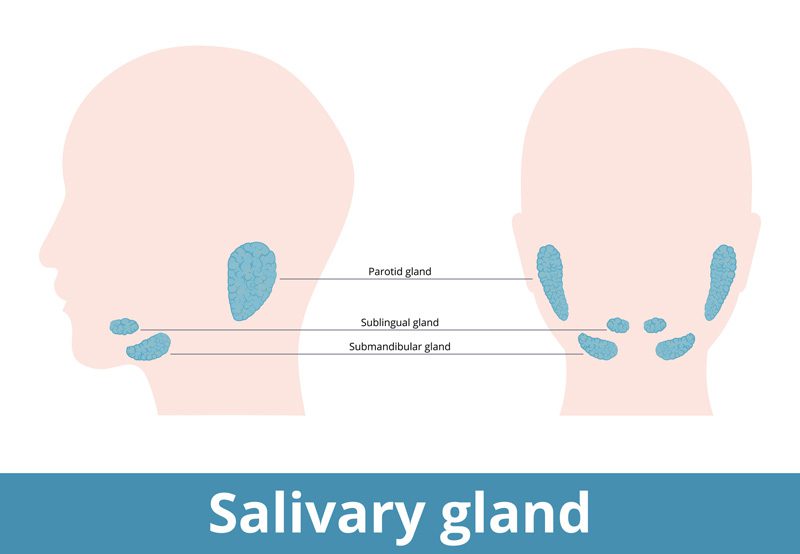

The human salivary system, composed of both major and minor salivary glands, plays an integral role in the proper functioning of the oral cavity. It not only aids in the initial digestion of food but also maintains oral hygiene and moisture. Sometimes, however, complications arise, such as obstructions or infections, which can hinder the gland’s optimal operation. In such situations, salivary gland endoscopy becomes an invaluable diagnostic and therapeutic tool.
What is Salivary Gland Endoscopy?
Salivary gland endoscopy, also known as sialendoscopy, is a minimally invasive procedure used to diagnose and treat conditions associated with the salivary glands. This procedure involves inserting a thin, flexible tube with a light and camera into the ducts of the salivary gland. It provides a direct visualization of the ductal system, allowing for the precise identification and management of abnormalities.

Why is it Needed?
Several conditions can affect the salivary glands, including:
- Salivary stones or sialoliths: Hardened mineral deposits that can block the flow of saliva.
- Stenosis: Narrowing of the ducts that can lead to reduced saliva flow and recurrent infections.
- Infections: Often caused by bacteria, which can result in pain and swelling.
- Duct inflammation secondary to radioactive iodine treatment or autoimmune diseases (Sjogren’s disease)
By utilizing salivary gland endoscopy, healthcare professionals can accurately diagnose these issues and decide on the best treatment pathway.
Benefits and Advantages
One of the primary advantages of this procedure is its minimally invasive nature. Traditional methods for addressing salivary gland problems often involved more invasive surgeries that might require external incisions and longer recovery times. Sialendoscopy, on the other hand, doesn’t typically require any external incisions, leading to less post-operative discomfort and faster recovery.
Moreover, it provides real-time visualization, which is crucial for both diagnosis and treatment. For instance, if a salivary stone is identified, it can often be removed during the same procedure.
What to Expect During The Procedure
The process begins with a local anesthetic to numb the area. Once the patient is comfortable, the endoscope is carefully inserted into the affected salivary gland’s duct. This provides a clear view of the interior, allowing the physician to identify any abnormalities.
If therapeutic intervention is required, specialized micro-instruments can be introduced through the endoscope. This might involve breaking up and extracting stones, dilating narrowed ducts, or flushing out the gland to clear infections.
Post-procedure, patients are typically observed for a short period to ensure there are no immediate complications. Most patients can return to their regular activities soon after, although some might experience minor discomfort, swelling, or transient salivary changes.
Potential Risks and Complications
Like all medical procedures, sialendoscopy is not without risks. Some potential complications include:
- Injury to the salivary duct or gland
- Infection
- Incomplete removal of obstructions
- Swelling or inflammation post-procedure
However, in the hands of skilled professionals, these risks are minimal. It’s always important for patients to discuss potential risks and benefits with their healthcare provider before undergoing the procedure.
Overview of Salivary Gland Endoscopy
Salivary gland endoscopy represents a significant advancement in the realm of otolaryngology, providing a minimally invasive solution to diagnose and treat salivary gland conditions. With its ability to reduce recovery times and increase diagnostic accuracy, it has become a preferred method for many healthcare providers and patients alike. As with any medical procedure, it’s essential to consult with a trusted otolaryngologist to determine the best course of action based on individual circumstances.
